
Breast cancer refers to a group of diseases where changes in the DNA of cells in breast tissue lead to uncontrolled growth. Such uncontrolled growth usually forms lumps that are either palpable (can be felt) or visible on X-Ray.
Invasive breast cancers usually start in the ducts that carry milk to the nipple (ductal carcinoma) or glands that form milk (lobular carcinoma). Ductal carcinoma in-situ (DCIS) is a form of breast cancer that is a precursor to invasive cancer.
Breast cancers are caused by DNA changes that lead to uncontrolled growth of cells in breast tissue. Most of these DNA changes are sporadic occurrences that cannot be predicted reliably. An inherited genetic predisposition may be found in less than 10% of all breast cancer cases.
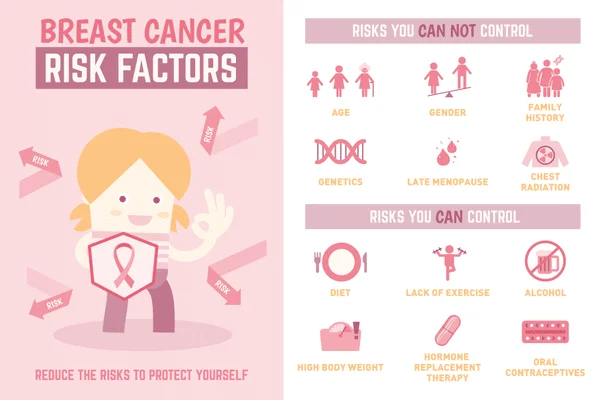
Having certain risk factors increases your chances of developing breast cancers, but it does not mean you will get the disease.
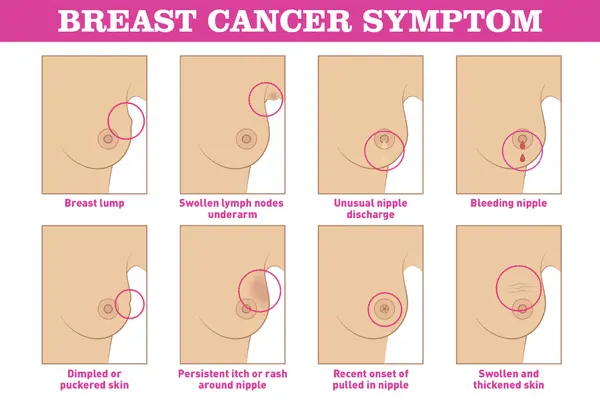
Breast cancer screening allows cancer detection before it causes symptoms (like a lump that can be felt). Breast cancers found during screening exams are more likely to be smaller and at an earlier stage. The size of a breast cancer and extent of spread to neighbouring lymph nodes are some of the most important factors in predicting the prognosis (outlook) of a woman with this disease.

Most masses seen on mammograms are benign (not cancerous). When a cancer is suspected, a needle biopsy of the breast mass is required to obtain tissue for microscopic analysis. Additional biopsy and placement of small marking clips inside the breast tissue (to locate the area of concern) may be required to confirm if enlarged/suspicious lymph nodes under the arm have been affected by the cancer.
Upon confirmation of the breast cancer diagnosis, additional testing will be performed to understand the subtype, tumour grading, expression of hormone receptors (estrogen and progesterone) and HER2 protein. These factors will aid the breast cancer specialist in creating a management plan for the patient.
Except for very small breast cancers, patients should undergo additional staging scans to determine the extent (or spread) of the cancer. Imaging that may be used include CT (computed tomography), bone scan, PET or MRI.
At The Cancer Centre, treatment of breast cancers largely depend on the stage of the cancer, hormone receptors/HER2 expression, the patient’s wish and health comorbidities (presence of other existing disorders).
Breast Cancer Treatment Based on Cancer Stage:
As oncologists, we work very closely with breast surgeons and plastic surgeons to achieve the optimal oncological and cosmetic outcomes for our patients. Here are the different types of surgeries for treating breast cancer:
For early stage breast cancers:
Neoadjuvant (prior to surgery) or adjuvant (after surgery) drug treatment may be offered to reduce the risk of cancer relapse and improve the chance of cure.
Recent advancements has seen the use of genomic profiling, particularly in tumours without HER2 protein overexpression, to better select patients who will benefit from adjuvant chemotherapy, and to avoid using chemotherapy in patients with lower risks of recurrence.
For metastatic breast cancers:
Drug selection depends on hormone expression, HER2 protein overexpression and other newer molecular markers in order to optimise quality of life and survival.
Chemotherapy refers to anti-cancer drugs that work in various ways to kill cancer cells. . There are many chemotherapy drugs that are effective for breast cancer. Most of them are in intravenous (IV) formulations but there are oral formulations as well.
Depending on the breast cancer state, chemotherapy may sometimes be given together with surgery, or at other times given alone without surgery.
Chemotherapy is given in varying cycles (schedules), typically as an injection every 1–4 weeks. Occasionally, chemotherapy is given in a metronomic schedule (continuous dosing of low doses) to improve tolerance towards the medication.
The side effects of chemotherapy vary; not all drugs lead to hair loss, severe vomiting or major impairment in the immune system. Your oncologist will be able to manage and guide you through the chemotherapy side effects with supportive medications.
 b). Hormonal Therapy
b). Hormonal Therapy2 in 3 breast cancer patients have receptors that are stimulated by naturally occurring female hormones (estrogen and progesterone). For these women, hormonal therapy blocks the interaction between their female hormones and these receptors.
Hormonal treatment can be used in the adjuvant setting (after surgery) for 5–10 years or for cases that have relapsed. Aromatase inhibitors and Fulvestrant are approved to be used in a post-menopausal setting, whereas Tamoxifen can be used in both pre and post-menopausal settings. These drugs have slightly different side effect profiles and patients who are intolerant to one drug may switch out to another drug for better tolerance.
Some breast cancer cells have dominant gene mutations driving the growth of the cancer. Discovery and understanding of these mutations have led to the development of drugs that specifically block these mutations:

Radiotherapy is treatment with high-energy rays to destroy cancer cells.
Adjuvant radiotherapy to reduce risk of local recurrence is recommended for women with:
Breast cancer is the most common cancer in Singaporean females. However, breast cancer screening helps detect the cancer at an earlier stage and saves lives. There have also been major advancements in breast cancer treatment with a better selection of tools, more targeted drugs for improved efficacy and reduced side effects, more modern surgical and radiotherapy techniques and better supportive care.
Visit The Cancer Centre in Singapore for breast cancer screening and treatment options.
Sources:
The Cancer Centre @ Mount Elizabeth Orchard
3 Mount Elizabeth #03-04
Mount Elizabeth Medical Centre
Singapore 228510

BOOK AN APPOINTMENT
Được thành lập vào năm 2005, Tập đoàn Y tế Singapore (SMG) là một tổ chức chăm sóc sức khỏe với mạng lưới các nhà cung cấp chuyên khoa tư nhân trên bốn trụ cột đã được thiết lập - Thẩm mỹ, Chẩn đoán hình ảnh & Sàng lọc, Ung thư và Sức khỏe Phụ nữ và Trẻ em. Tại Singapore, SMG có hơn 40 phòng khám có vị trí chiến lược ở trung tâm Singapore và các khu trung tâm. Ngoài Singapore, SMG cũng đã có mặt tại Indonesia, Việt Nam và Úc. Tìm hiểu về chính sách bảo mật của chúng tôi tại đây.
